Dental related conditions
What has functional breathing got to do with oral health?
It might be a surprise to learn that normal breathing has a huge effect on oral health. The following conditions are related to dysfunctional breathing:
-
- Dental crowding and malocclusion (misalignment of the teeth when the jaw closes)
- Dry mouth, gum disease and dental decay
Dental Crowding and Malocclusion
Dental crowding appears to be as common as dysfunctional breathing. Mouth breathing is a major cause of dental crowding due to the fact that the tongue sits too low when we breathe through our mouths.

The majority of children today exhibit some degree of malocclusion (crooked teeth and jaws)1, 2 and it has been well documented that this is related to soft tissue dysfunction.3,4 In fact, it is now well accepted that the muscles of the tongue, lips and cheeks play a major role in tooth position and jaw development.5,6
Relevant literature explains how mouth breathing is a significant factor in the aetiology of malocclusion.7, 8, 9, 10, 11, 12 In short, when mouth breathing occurs, the tongue moves down in the mouth to allow the passage of air above it. An open mouth posture affects the direction of growth of the face/head as the muscles pulling on the jaws are affected. Breathing through the mouth causes the tongue to sit lower as well as altering the head and neck posture. This low tongue posture then leads to reduced maxillary growth13, 14 and increases the vertical growth of the face, as opposed to a broad jaw development.
References for the above text:
1 Prevalence of malocclusion and orthodontic treatment need in children and adolescents in bogota, Columbia. Birgit Thilander, Lucia Pena, Clementina Infante, Sara Stella Parada, Clara de Mayorga. European Journal of Orthodontics.
2 Prevalence and distribution by gender of occlusal characteristics in a sample of Italian secondary school students: a crosssectional study. Fabio Ciuffolo, Lamberta Manzoli, Michele D’Attilo, Simona Tecco, Filippo Muratore, Felice Festa, Ferdinando Romano. European Journal of Orthodontics.
3 Soft Tissue Dysfunction: a missing clue when treating malocclusions. German O. Ramirez- Yanez, Chris Farrell. International Journal of Functional Orthopedics (2005).
4 Muscling in on the truth. Rohan Wijey. Australasian Dental Practice.
5 Insights into Orthodontic Treatment. German O. Ramirez-Yanez. Dental Asia (July/August 2006).
6 The Trainer System in the context of treating malocclusions. German O. Ramirez-Yanez. Ortho Tribune (August / September 2009).
7 Mouth breathing in allergic children: Its relationship to dentofacial development. Dante Bresolin, D.D.S., M.S.D., Peter A.Sharpiro, D.D.S., M.S.D., Gail G. Shapiro, G.M.D., Chapko, M.K. Ph. D., and Dassel, S. M.D. Brasilia, D.F., Brazil, and Seattle, Wash. American Journal of Orthodontics and Dentofacial Orthopedics 1983.
8 Prevalence of malocclusion among mouth breathing children: do expectations meet reality? Souki BQ, Pimenta GB, Souki
MQ, Franco LP, Becker HM, Pinto JA, Federal University of Minas Gerais, Outpatient Clinic for Mouth-Breathers, Belo Horizonte, Brazil. Int J Pediatr Otorhinolaryngol. 2009 May; 73(5): p.767-773.
9 Etiology, clinical manifestations and concurrent findings in mouth-breathing children. Abreu RR, Rocha RL, Lamounier JA, Guerra AF. J Pediatr (Rio J). 2008 Nov-Dec; 84(6): p.529-535.
10 Radiological evaluation of facial types in mouth breathing children: a retrospective study. Costa JR, Pereira SR, Weckx LL, Pignatari SN, Uema SF. Int J Orthod Milwaukee. 2008 Winter; 19(4): p. 13-16.
11 The negative effect of mouth breathing on the body and development of the child. Flutter J. Int J Orthod Milwaukee. 2006 Summer; 17(2): p. 31-37.
12 Nasal Obstruction and Facial Growth: The Strength of Evidence for Clinical Assumptions. Katherine W. L. Vig, BDS, MS, FDS, DOrth. Dentofacial Ortholi 1998; 113:663-11.
13 Insights into Orthodontic Treatment. German O. Ramirez-Yanez. Dental Asia (July/August 2006).
14 The Trainer System in the context of treating malocclusions. German O. Ramirez-Yanez. Ortho Tribune (August / September 2009).

Dry mouth, gum disease and dental decay
Saliva coats and lubricates tissues in the mouth, making it easier to speak, chew and swallow. Furthermore, it helps remove oral waste and cavity-causing bacteria, and protects teeth from decay by neutralising harmful acids; saliva also helps remineralise tooth enamel.
If your habitual breathing pattern is through your mouth, it is more likely that you will suffer from a dry mouth, and will not benefit so much from the normal protective functions of saliva. By learning to comfortably and gently breathe through your nose with your lips together using the BIM, you will be assisted in maintaining a normal healthy oral environment.
COPD (Chronic Obstructive Pulmonary Disease), Emphysema and Breathlessness

A diagnosis of COPD and emphysema indicates that damage has occurred to the delicate tissues of the lung – the alveoli. These small, elastic walled air sacs in the lungs are critical to efficient oxygen exchange. The severity of the condition will depend on the extent of damage to the alveoli.
The chief symptom of emphysema is breathlessness and fatigue during any activity. Despite the lung damage, it may be possible through breathing retraining to improve the mechanics and efficiency of breathing, both when at rest and during activity. Many BIM clients with emphysema report a reduction in mucous production, less breathlessness and that the techniques learnt help them to improve their quality of life.
Chronic Fatigue Syndrome / ME
Often there is no apparent cause for this very debilitating condition, in which many people suffer from chronic exhaustion and muscle and joint pains, regardless of the amount of sleep or rest. Improving a dysfunctional breathing pattern may assist in improving oxygenation to the cells and tissues of the body. Some people suffering from this condition have been able to achieve improvement in their health and increased energy levels through learning the BIM.
As the above MRI scan shows, oxygenation to the brain was decreased by 40% through just one minute of over-breathing. If someone is over-breathing 24/7 then they will have less than optimum oxygenation of the cells throughout the body. Oxygen appropriate to our metabolic needs is necessary for energy. If we are not breathing properly, or more specifically if we are over-breathing we will be in this low oxygen environment; this may cause us to feel tired, groggy and always low on energy.
In addition to that people who have dysfunctional breathing patterns tend to sleep poorly i.e. snoring, sleep apnoea or just not getting a restful sleep. Poor breathing keeps us sympathetic dominant (fight or flight branch of the nervous system). If we are sympathetic dominant we are less likely to sleep deeply and restfully, further compounding low energy levels.
BIM breathing exercises and lifestyle changes are aimed at restoring normal breathing patterns. This may lead to a stabilising of the blood pH, better hormonal level and function, more refreshing sleep, and reduction in allergic responses thus lessening the load on the body’s energy resources.
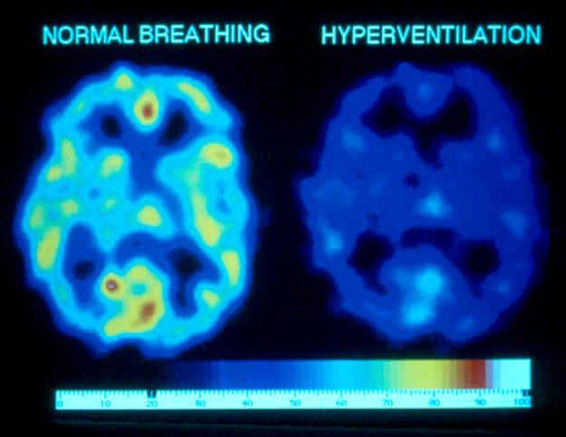
Over breathing and CO2 loss reduces brain oxygenation
MRI SCAN
red – yellow = highest oxygen
dark blue = least oxygen
The right hand image shows a 40% reduction in brain oxygen after one minute of big volume breathing. (source Litchfield 1999)



